Peritonsillar Abscess
What's a Peritonsillar Abscess?
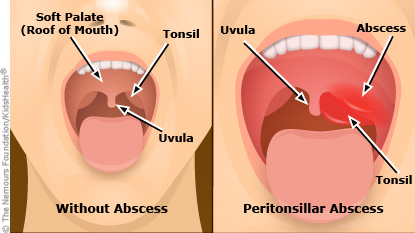
A peritonsillar abscess is an area of pus-filled tissue at the back of the mouth, next to one of the tonsils. The abscess can be very painful and make it hard to open the mouth.
It can also cause swelling that can push the tonsil toward the uvula (the dangling fleshy object at the back of the mouth). This can block the throat, making it hard to swallow, speak, and sometimes even breathe.
An abscess that's not promptly treated can lead to a spread of the infection into the neck and chest, and other serious problems.
What Causes a Peritonsillar Abscess?
Most peritonsillar abscesses are caused by the same bacteria (group A streptococcus) that cause strep throat. Sometimes other types of bacteria are also involved.
Peritonsillar abscesses usually happen as a complication of tonsillitis, when the infection spreads from a tonsil into the space around it. Fortunately, these kinds of abscesses are uncommon because doctors use antibiotics to treat tonsillitis.
Periodontal (gum) disease and smoking can increase a person's chances of developing an abscess.
What Are the Signs of a Peritonsillar Abscess?
The first sign of a peritonsillar abscess usually is a sore throat. As the abscess develops, other symptoms start, such as:
- red, swollen tonsils
- tender, swollen glands (lymph nodes) on one side of the neck
- severe pain on one side of the throat
- difficulty and pain when swallowing or opening the mouth
- fever and chills
- headache
- earache
- drooling
- a muffled or hoarse voice
- bad breath
An abscess that goes untreated for a long time can lead to serious problems — for example, the infection may spread into the jaw, neck, and chest. If the abscess ruptures, the infection may lead to pneumonia.
How Is a Peritonsillar Abscess Diagnosed?
Call a doctor if your child has a sore throat along with a fever or any of the other symptoms of a peritonsillar abscess. It's rare that an abscess will restrict breathing, but if it does, you might need to take your child to the emergency room right away.
The doctor will examine your child's mouth, throat, and neck. They will look for an extremely swollen red area around the tonsil that pushes against the uvula. The doctor also might do a throat culture and a blood test. Rarely, a doctor may order a CT scan or ultrasound to help make the diagnosis.
How Is a Peritonsillar Abscess Treated?
The usual treatment for a peritonsillar abscess involves draining it. The doctor withdraws the pus with a needle (called aspiration) or makes a small cut in the abscess with a scalpel so the pus can drain out.
If this doesn't work, the tonsils might need to be removed in a tonsillectomy. This is especially true for kids who have had multiple recent cases of tonsillitis or a prior peritonsillar abscess.
Kids who have a tonsillectomy may need a brief stay in the hospital. That way, doctors can keep an eye on them to make sure everything went as planned.
The doctor will prescribe pain relievers and antibiotics. Make sure your child finishes all the antibiotics, even if they feel better after a few days. Otherwise, the infection could come back.
The quicker a peritonsillar abscess is diagnosed, the easier it is to treat. So if you notice symptoms, call your doctor right away.
Can Peritonsillar Abscesses Be Prevented?
Good oral hygiene can help kids avoid getting a peritonsillar abscess. And teens shouldn't smoke because, among other health risks, smoking can make them more likely to develop an abscess.


